This webpage is available for historical purposes. It is no longer being updated and may not reflect current guidance. For current guidance see:
12-13-22
11-21-22
The LA County Health Officer orders require persons diagnosed with COVID-19 to isolate and their close contacts to follow Instructions for Close Contacts. See Quick Links to view Health Officer Orders and Instructions.
Healthcare providers who diagnose a patient with COVID-19 (confirmed or presumed) are asked to give their patient isolation orders and instructions and to provide their close contacts with instructions (available at ph.lacounty.gov/covidcontacts).
Providers should have a low threshold to prescribe COVID-19 therapeutics to infected patients given the broad range of individuals who are at higher risk for severe COVID-19 who may benefit from COVID-19 outpatient treatment. In addition, providers are encouraged to proactively tell patients who are close contacts about how to access outpatient treatment quickly should they test positive and have symptoms. Learn more at ph.lacounty.gov/covidtherapeutics
When COVID-19 is confirmed or presumed, the diagnosing provider is asked to:
Antiviral Therapy for Ambulatory Patients
Early outpatient treatment of COVID-19 can avert serious, potentially life-threatening illness. Healthcare providers should prescribe COVID-19 treatment to the extent possible to outpatients who meet all of the following:
See COVID-19 Therapy for Non-Hospitalized Patients at ph.lacounty.gov/covidtherapeutics for currently recommended treatments.
Symptomatic COVID-19 Infection
Isolation can end after Day 5 ONLY if all of the following criteria are met:
--or--
Isolation can end after Day 10 if fever-free for 24 hours without the use of fever-reducing medications. If fever is present, isolation should continue until 24 hours after fever resolves.
Note: Most outpatients with follow-up positive viral tests may end isolation after Day 10. This is because patients who have recovered from COVID-19 can continue to have positive COVID-19 viral tests when they are no longer infectious. CDC recommends extending isolation for patients who were severely ill or who are moderately to severely immunocompromised. See Severe/Critical COVID-19 or Immunocompromised.
Patients with an initial presumptive clinical diagnosis of COVID-19 who are ruled out—if the healthcare provider reassesses the initial diagnosis and concludes that the patient is not infected with SARS-CoV-2 (and they never tested positive), the patient can leave isolation after they have been fever-free for 24 hours. If they are close contacts they must continue to follow instructions for close contacts.
Asymptomatic COVID-19 Infection
Persons with COVID-19 who never developed symptoms may be released from isolation:
After Day 5 if they have a negative COVID-19 viral test result from a specimen collected on Day 5 or later (antigen test preferred).
--or--
After Day 10 from the date of collection of the initial positive viral test.
Note: Most outpatients with follow-up positive viral tests may end isolation after Day 10. This is because patients who have recovered from COVID-19 can continue to have positive COVID-19 tests in upper respiratory specimens for up to 3 months after initial illness. CDC recommends extending isolation for patients who were severely ill or are immunocompromised. See Patients Who Are Immunocompromised or Had Severe/Critical COVID-19 Illness next.
Patients Who Are Immunocompromised or Had Severe/Critical COVID-19 Illness
For patients with severe to critical COVID-19 illness (e.g., required hospitalization, intensive care, or ventilation support) who are not immunocompromised, the CDC recommends extending the duration of isolation and precautions from 10 days to up to 20 days from illness onset. This is because they may produce replication-competent virus beyond 10 days.
For patients who are moderately to severely immunocompromised (regardless of symptoms or COVID-19 illness severity) the CDC recommends an isolation period of at least 20 days, ending isolation in conjunction with a test-based strategy and consultation with an infectious disease specialist to determine the appropriate duration of isolation and precautions. This is because moderately or severely immunocompromised patients may produce replication-competent virus beyond 20 days.
See CDC Interim Guidance on Ending Isolation and Precautions for Adults with COVID-19 for more details.
Generally, employers may determine if their employees/contractors with COVID-19 must complete the full 10 days of isolation before returning to work or if they may return to work after Day 5 if the criteria above are met. Employees/contractors are advised to obtain information from their employer.
Children may return to school when they have completed isolation. For more information, refer to ph.lacounty.gov/EducationToolkitTK12.
Asymptomatic close contacts are no longer are required to quarantine, regardless of vaccination status.
Asymptomatic close contacts in the general public do not need to quarantine. They must follow all instructions at ph.lacounty.gov/covidcontacts.
All close contacts in the general public are required to:
If they test positive at any time, they must follow isolation requirements at ph.lacounty.gov/covidisolation. See section above: Isolation-COVID-19 in Ambulatory Patients
*If the close contact is at increased risk for severe illness or if they live with someone at higher risk for severe illness, testing is recommended as soon as possible and, if negative, again on Day 5. Identifying infection early after exposure enables earlier access to outpatient treatment options should symptoms be detected.
Providers are asked to tell their patients who are close contacts about outpatient treatments for COVID-19 should they test positive for COVID-19 and develop any symptoms. Please note that the majority of adults and some children with COVID-19 are eligible for treatment including people who are not up to date with COVID vaccinations, people in a racial or ethnic minority group, people with disabilities and common conditions including obesity, depression, smoking (former or present), and physical inactivity. See full CDC list. Please emphasize the importance of starting therapy soon after symptoms start and tell them how to contact your office for a prescription/referral if appropriate. See ph.lacounty.gov/covidtherapeutics
Certain high-risk settings may require additional precautions. See sector specific guidance for further information:
A patient with a history of recent recovery from COVID-19 is defined as a person with a positive viral COVID-19 test within the past 3 months (90 days) who has recovered from the previous infection. Recovered means they are no longer considered infectious (i.e., their isolation period has ended).
If the patient had symptoms with their most recent infection, the 90 days are from the onset of the initial COVID-19 symptoms. If they never had symptoms, then the 90 days are from the date of collection of the first positive viral COVID-19 test.
If the recently recovered person
Is asymptomatic:
Develops new symptoms consistent with COVID-19 illness:
Rationale:
Immunocompetent patients who have recovered from acute COVID-19 infection can continue to have detectable SARS-CoV-2 RNA in upper respiratory specimens for 3 months after illness onset and persistent positive antigen tests are possible for at least 24 days. Replication-competent virus has not been reliably recovered from such patients, and they are not likely infectious.
Antigen testing of asymptomatic close contacts is recommended to identify a new infection if 31-90 days have passed since their first positive test. This is because persistent antigen positivity is unlikely after a month and because the probability of SARS-CoV-2 reinfection increases with time due to exposure to viral variants and waning immunity.
See CDC Key Findings from Transmission Literature for more information.
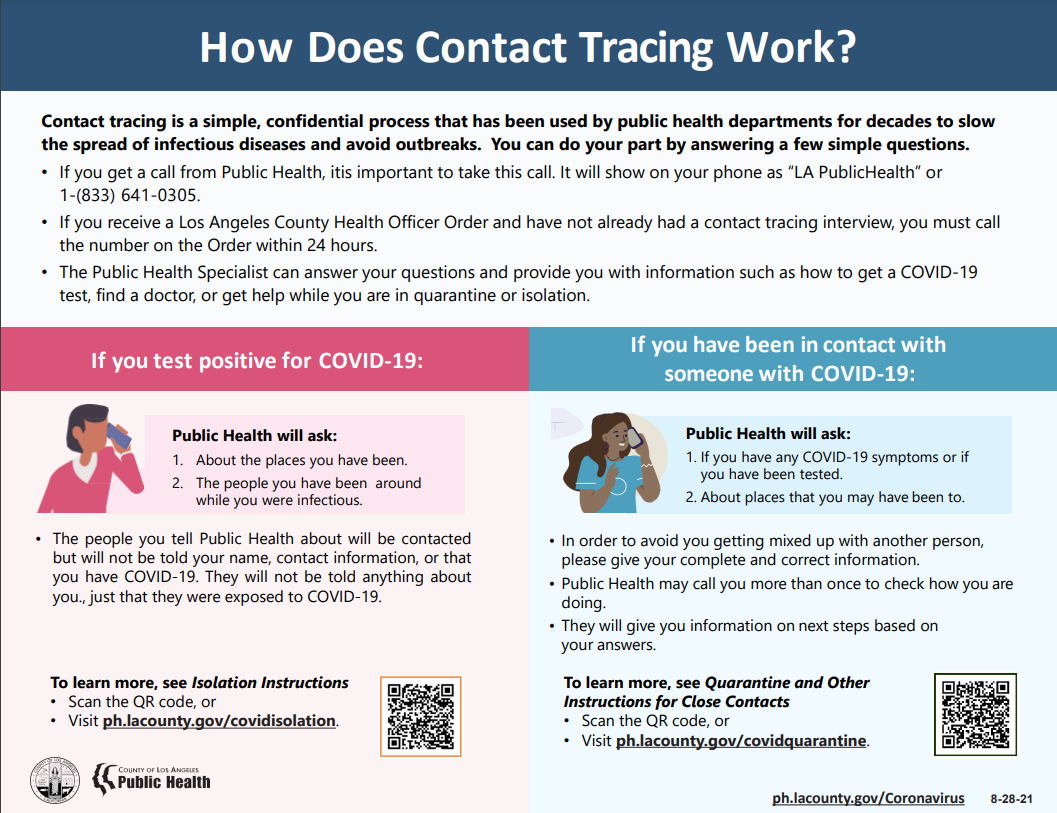
LAC DPH will attempt to contact patients with COVID-19 by phone or text. LA County Public Health staff will answer any questions the patient may have and share helpful resources.
This flyer explains to patients what to expect.
Resources for patients —the patient isolation and instructions for close contacts are available on webpages in English and Spanish and in PDFs in 13 languages. They also host resources including:
Visit home isolation and instructions for close contacts to view these resources.
Short URLs - are available at the top of this page to make it easier to direct patients to the quarantine and isolation webpages over the phone.
Information about symptoms - information from DPH (ph.lacounty.gov/covidcare) and the CDC for people who want to learn about symptoms, or who have symptoms of COVID-19 but have not been tested or sought medical advice.
Additional information for providers in multiple languages is available on the LAC DPH Print materials webpage.