Our Reports
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2017-2023
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2017-2023 (March 2025)
This is our sixth annual report on mortality rates and causes of death among people experiencing homelessness (PEH) in LA County. 2023 marked the second year in a row that the mortality rate among PEH in LA County remained high but stable, after two years of alarming increases from 2019 to 2021. Those earlier increases were driven primarily by a rapid rise in fentanyl overdoses, but also by the COVID-19 pandemic and notable increases in transportation-related injury deaths and homicides. Despite a continued rise in drug overdose mortality in 2022, that year saw the beginning of the current plateau in overall mortality, due to a sharp drop-off in COVID-19 deaths and a stabilization of deaths from transportation-related injuries. The continued plateau in overall mortality in 2023 was driven by a leveling-off of drug overdose mortality that year, despite an increase in coronary heart disease (CHD) mortality and a decrease in homicide mortality. Transportation-related injury mortality remained high but stable in 2023.
Your feedback is important to us.
Please take a moment to answer
these 3 questions.
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2014-2022
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2014-2022 (May 2024)
This is our fifth annual report on mortality rates and causes of death among people experiencing homelessness in LA County. We found that the mortality rate plateaued in 2022, after two years of alarming increases. We are cautiously optimistic about this finding because one year does not yet constitute a trend, and the mortality rate is still unacceptably high. The recent leveling off of the overall mortality rate was largely driven by plateaus in the overdose and traffic-related mortality rates along with a sharp decline in COVID-19 mortality. A substantial 2022 increase in the distribution of naloxone, an opioid overdose reversal medication, likely contributed to the flattening of the overdose mortality curve. Despite the leveling off the overdose mortality rate, the proportion of overdose deaths involving fentanyl continued to rise in 2022 to 66%. In 2021 and 2022 combined, the mortality rate among people experiencing homelessness was about 4 times greater than among all LA County residents. We recommend expanded access to housing and shelter, along with physical, mental and behavioral health and harm reductions services tailored to the needs and circumstances of people experiencing homelessness as critical strategies for reducing mortality in this vulnerable population.
Medical Debt in Los Angeles County Baseline Report and Action Plan:2023
Medical Debt in Los Angeles County Baseline Report and Action Plan:2023
This is a baseline report on medical debt burden in Los Angeles (LA) County based on an analysis conducted by the LA County Department of Public Health (Public Health) using data from the California Health Interview survey. Approximately one is ten LA County adults—about 810,000 people—had problematic medical debt as of 2021, for a total of over $2.6 billion in outstanding medical debt. Those most effected by medical debt included Latino, Black, and American Indian, Pacific Islander, or mixed-race adults, families with children, low-income families, and low-income families. People with medical debt were more likely to forgo needed medical services and prescriptions and were more likely to experience unstable housing and food insecurity, thus undermining the social conditions necessary for improving public health. To address this complex challenge, Public Health has established a diverse coalition of medical debt stakeholders, including consumers, nonprofit organizations, policy experts, and healthcare leaders. This group has provided Public Health with key recommendations for appropriate County-level action. Continued collaboration is essential to effectively tackle the medical debt crisis in LA County.
Medical Debt in Los Angeles County Baseline Report and Action Plan:2023 Report
![]()
Deuda Médica en el Condado de Los Ángeles: Informe de Referencia y Plan de Acción Junio de 2023
Deuda Médica en el Condado de Los Ángeles: Informe de Referencia y Plan de Acción Junio de 2023
Este es el primer reporte sobre la deuda médica en el condado de Los Angeles, llevado a cabo por el departamento de salud pública del condado, usando datos del California Health Interview Survey. Aproximadamente uno de cada diez adultos, o alrededor de 810,000 residentes, están afectados, con más de $ 2.6 mil millones en deuda médica pendiente a partir de 2021. Los latinos están particularmente afectados, tal como las familias con niños y la gente pobre. Los adultos con deudas médicas eran tres veces más propensos a saltarse o retrasar la atención sanitaria necesaria, y tres veces y media más propensos a retrasar o no recoger las recetas en comparación con los que no tenían deudas médicas.
Deuda Médica en el Condado de Los Ángeles: Informe de Referencia y Plan de Acción Junio de 2023
![]()
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2014-2021
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2014-2021 (May 2023)
This is our fourth annual report on mortality rates and causes of death among people experiencing homelessness (PEH) in LA County. We found that the PEH mortality rate increased sharply during the first two years of the COVID-19 pandemic (2020-21). This increase was attributed largely to increases in drug overdose deaths, as well as traffic injury and homicide deaths. Fentanyl was the drug most responsible for the increase in overdose deaths. The percentage of PEH deaths with fentanyl involvement tripled from 2019 to 2021. COVID-19 became the fifth leading cause of death among PEH, and the COVID-19 mortality rate was 1.8 times greater among PEH compared to the LA County population in 2020-21 combined. However, the mortality gap was considerably higher for other causes of death. During those same years, the drug overdose mortality rate was 38.9 times greater among PEH compared to the public, and traffic injury and homicide mortality rates were 20.4 and 15.1 times greater among PEH, respectively.
Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County:2014-2021 Report
![]()
Download Infographics 2023 ![]()
Issue Brief: Mortality among People Experiencing Homelessness in Los Angeles County: One Year Before and After the Start of the COVID-19 Pandemic
Mortality among People Experiencing Homelessness in Los Angeles County: One Year Before and After the Start of the COVID-19 Pandemic (April 2022)
This report compares deaths among people experiencing homelessness during the 12-month periods preceding and following the first reported PEH COVID-19 death in LA County. The overall number of deaths among PEH increased by 56%, from 1,271 to 1,988 deaths, between the two 12-month periods. During the post-pandemic onset period there were 179 COVID-19 deaths among PEH, accounting for 25% of the observed increase. Excluding these deaths, the number of deaths among PEH still increased by 43%.
Brief: Mortality among People Experiencing Homelessness in Los Angeles County: One Year Before and After the Start of the COVID-19 Pandemic
![]()
Download Homeless Report 2022 Toolkit ![]()
Issue Brief: Recent Trends in Mortality Rates and Causes of Death Among People Experiencing Homelessness
Recent Trends in Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County (January 2021)
After steadily increasing by over 30% between 2014 and 2018, the overall mortality rate among people experiencing homelessness (PEH) in LA County rose only slightly in 2019 compared to the previous year. This flattening of the overall curve was due to an increase in the homeless population that kept pace with the increase in the number of deaths, which rose to a record total of 1,267 in 2019. Despite the relatively small increase in the overall mortality rate, the rate of drug overdose deaths continued to increase substantially among PEH in 2019. The drug type involved in the highest percentage of overdose deaths in 2018, 2019 and the first seven months of 2020 was methamphetamine, but the only drug involved in increasing percentages of overdose deaths across all three years was fentanyl, which was involved in more than twice as many overdose deaths in the first seven months of 2020 as in all of 2019.
Brief: Recent Trends in Mortality Rates and Causes of Death Among People Experiencing Homelessness
![]()
Issue Brief: Vaping Risks, Behaviors, and Policy Responses
Vaping Risks, Behaviors, and Policy Responses: A View from Los Angeles County
This issue brief summarizes what we know about the recent e-cigarette, or vaping, associated lung injury (EVALI) outbreak, and rising rates of nicotine vaping among youth in LA County and across the country. The US Centers for Disease Control and Prevention has strongly linked vitamin E acetate found in THC vaping products to the EVALI outbreak, though there is not yet enough evidence to rule out other potential chemicals of concern or non-THC vaping products. Even before the recent EVALI outbreak began in California in June 2019, middle and high schoolers' use of e-cigarettes had dramatically increased across the US. Due to a history of targeted public health policies LA County youth may have lower use rates than the rest of the country, but they are still unacceptably high. Levels of nicotine in e-cigarettes have increased and are now comparable to or greater than those found in cigarettes. Delays in FDA regulation have led to wide variation in product content which has made research on health effects challenging. However, we know that vaping nicotine can cause an increased heart rate, damage to cells that line blood vessels, and oxidative stress. We also know that among youth and young adults, e-cigarette use increases the risk of ever using cigarettes. To avoid unnecessary risk, refraining from all forms of vaping is recommended.
Issue Brief: Homeless Mortality
Recent Trends in Mortality Rates and Causes of Death Among People Experiencing Homelessness in Los Angeles County (October 2019)
This issue brief highlights data on homeless mortality, including leading causes of death and mortality rates by race/ethnicity and gender. Researchers found that the homeless mortality rate in LA County has been steadily increasing in recent years, driven primarily by drug or alcohol overdoses. After breaking down the data, the brief presents several recommendations that should help to reduce the mortality rate in this vulnerable population.
Issue Brief: Cannabis Premise Survey
Los Angeles County Cannabis Dispensary Premise Survey: Follow-up Survey of Licensed Dispensaries (September 2019)
This issue brief describes the second round of premise surveys that the Center conducted on 60 licensed dispensaries in June and July 2019, around the time that the below HIA on cannabis regulation was published. Topics for data collection included underage access, security, product types, promotional practices and neighborhood context. While the first round of premise surveys had focused on whether business practices differed between licensed and unlicensed dispensaries, this round focused on whether licensed dispensary business practices differed by the level of health advantage in their premise's neighborhood.
Brief: Cannabis Premise Survey
![]()
Journal Article - Assessing the Retail Environments of Licensed and Unlicensed Cannabis Dispensaries
![]()
Health Impact Assessment: Cannabis Regulation
Health Equity Impacts of Cannabis Regulation in Los Angeles County (July 2019)
This HIA assesses the health equity implications of local regulatory decisions regarding cannabis dispensary locations and business practices, regulatory enforcement and cannabis taxation. Based on extensive analyses of quantitative and qualitative data, the report includes 15 policy recommendations designed to provide a health equity lens for local jurisdiction considering whether and how to regulate cannabis in their areas.
Health Impact Assessment: Cannabis Regulation Report
![]()
Slides from Webinar
![]()
Download Webinar Recording
![]()
Health Brief: Cannabis Use
Recent Trends in Adult Use of Marijuana (July 2018)
This health brief describes rates of adult use of cannabis in Los Angeles County from 2005 to 2015, before the November 2016 passage of Proposition 64, the statewide initiative that legalized the cultivation, sale and use of cannabis (also referred to as marijuana). Data are from the Los Angeles County Health Survey, a periodic, population- based telephone survey that collects information on sociodemographic characteristics, health status, health behaviors, and access to health services among adults and children in the County. The brief also provides five key public health actions to minimize the adverse health impacts of cannabis legalization.
Health Impact Assessment: Mobility Plan
Implementing the City of LA's Mobility Plan 2035: Public Health Implications (May 2018)
The LA City Mobility Plan 2035 (MP) is designed to promote a balanced, multimodal transportation network that meets the needs of all users, including motorists, pedestrians, bicyclists, and users of public transportation. This HIA assesses the impacts of alternative future scenarios of MP implementation on deaths and disability from heart disease, stroke, diabetes, depression respiratory illness, and traffic injuries. Costs associated with these health outcomes are also estimated. Comprehensive implementation of the MP is associated with improvements in a variety of health outcomes and significant savings in health-related costs.
Health Impact Assessment: Mobility Plan Report
![]()
Journal Article - Routine Assessment of Health Impacts of Local TransportationPlans
![]()
Health Impact Assessment: Measure H
Health Impacts of Measure H: Preventing and Reducing Homelessness in Los Angeles County (February 2017)
This HIA assesses the housing and health impacts of Measure H, a ¼ cent sales tax initiative to fund homelessness services in LA County. We apply a public health lens to the Measure by organizing its various strategies according to three key populations at risk of homelessness and currently homeless. The HIA synthesizes research evidence for the housing and health impacts of Measure H strategies and provides recommendation for how to maximize these impacts through implementation, if the measure passes.
Health Impact Assessment: Measure H Report
![]()
Journal Article - Applying a prevention framework to address homelessness as a population health issue
![]()
Health Impact Assessment: Measure JJJ
Health Impacts of Initiative Ordinance JJJ: Affordable and Transit-Oriented Housing Policies for the City of Los Angeles (October 2016)
This HIA estimates the effects of Measure JJJ on affordable housing production and then examines the health impacts of affordable housing through decreases in rent burden, overcrowding and displacement, and increases in household proximity to transit, neighborhood integration and housing quality. The HIA offers recommendations that speak to the public health implications of affordable housing policies in general and suggests ways that the potential health benefits of Measure JJJ could be considered during the implementation process, if it passes.
Health Impact Assessment: Measure JJJ Report
![]()
Brief: Health Impacts of Initiative Ordinance JJJ
![]()
Summary (Spanish)
![]()
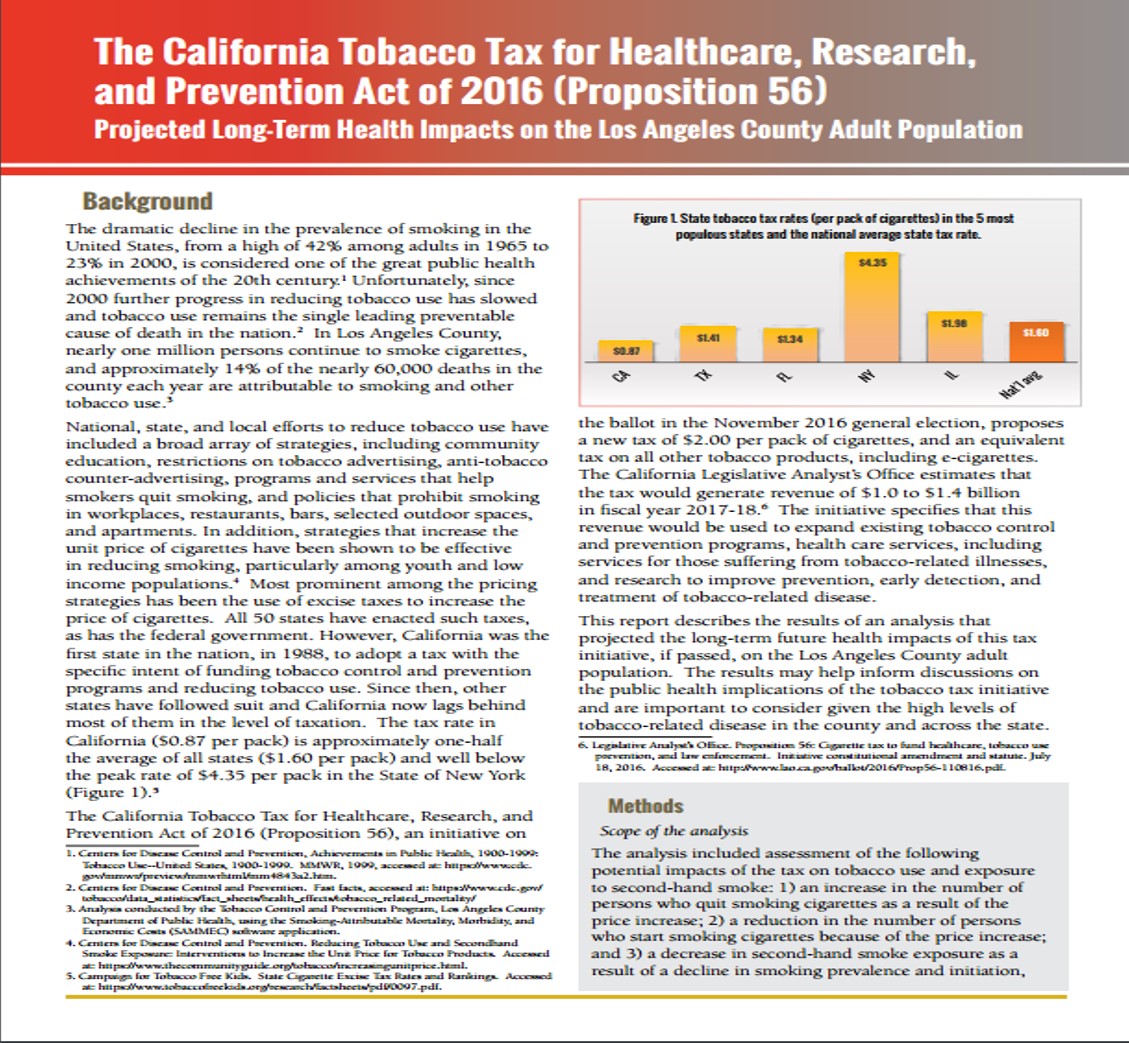
Issue Brief: Projected Long-Term Health Impacts of Proposition 56 on the Los Angeles County Adult Population
The California Tobacco Tax for Healthcare, Research, and Prevention Act of 2016
(Proposition 56): Projected Long-Term Health Impacts on the Los Angeles County
Adult Population
(October 2016)
This was a collaboration with the Division of Chronic Disease and Injury Prevention, with support
from the University of Southern California Schaeffer Center for Health Policy & Economics.
This report describes an analysis of the long-term health impact of Proposition 56 -
The California Tobacco Tax for Healthcare, Research, and Prevention Act of 2016. The
report was created by staff in the Office of Health Assessment and Epidemiology and
the Division of Chronic Disease and Injury Prevention, with support from the University
of Southern California Schaeffer Center for Health Policy & Economics. The findings
suggest that the tobacco tax specified in Proposition 56, if adopted and implemented,
would result in significant reductions in new cases of heart disease, stroke, chronic
lung disease, and cancer in the Los Angeles County adult population over the next four
decades. For more information about the design, methodology and results, click the
link below.
Issue Brief: Projected Long-Term Health Impacts of Proposition 56 on the Los Angeles County Adult Population
![]()
Toolkit: Rapid Health Impact Assessments
Guidance and Tools for Conducting Rapid Health Impact Assessments: Applying a Health Lens to Policy and Program Decisions in Los Angeles County, Version 1.2 (Updated July 2019)
The Center for Health Impact Evaluation at the Los Angeles County Department of
Public Health (LACDPH), developed a Rapid Health Impact Assessment Toolkit to
assist LACDPH staff, other local health agencies, and staff of agencies outside of the
health sector with guidance on when and how to conduct a 4-6 month HIA. This
document describes the six steps of the HIA process adapted to fit a more rapid time
frame. We've also developed a series of attachments to assist HIA practitioners when
they are conducting their RHIA, which include: 1) How to prioritize and screen
whether or not a RHIA should be conducted; 2) Tips and guidance for conducting a
RHIA; 3) Examples of pathway diagrams and policy briefs; 4) Available data sources
for conducting HIAs;
5) Effective stakeholder engagement methods; 6) Databases for
conducting literature reviews; and 7) Methods for tracking impact and outcome
indicators.
Rapid Health Impact Assessment: Second Chance Women's Re-Entry Court
Health and Public Safety Impacts of Sustaining a Women's Jail Diversion Program in Los
Angeles County: A Rapid Health Impact Assessment
(August 2015)
This was a collaboration with Los Angeles County District Attorney's Office, Public Defender,
Department of Probation, Superior Court, Prototypes, County Criminal Justice Coordination
Committee and DPH's Substance Abuse and Prevention Control Program.
The Center for Health Impact Evaluation at the Los Angeles County Department of Public Health, conducted a Rapid Health Impact Assessment to assess the impacts of a jail diversion program called Second Chance Women's Re-Entry Court. Women in the criminal justice system often suffer from mental health problems, chronic drug and alcohol addictions, and trauma histories. Diversion programs present an opportunity to address the complex needs of these women without some of the negative consequences associated with incarceration. This rapid HIA seeks to synthesize available data to assess the program’s impact on a variety of relevant outcomes, including recidivism, economic benefits of jail years saved, mental health, substance use, relationships, employment and housing stability among women charged with lower-level felonies (non-serious, non-violent, non-sex offender crimes). To access the full report and Executive Summary, please click on the links below.
Rapid Health Impact Assessment: Second Chance Women's Re-Entry Court Report
![]()
Executive Summary
![]()
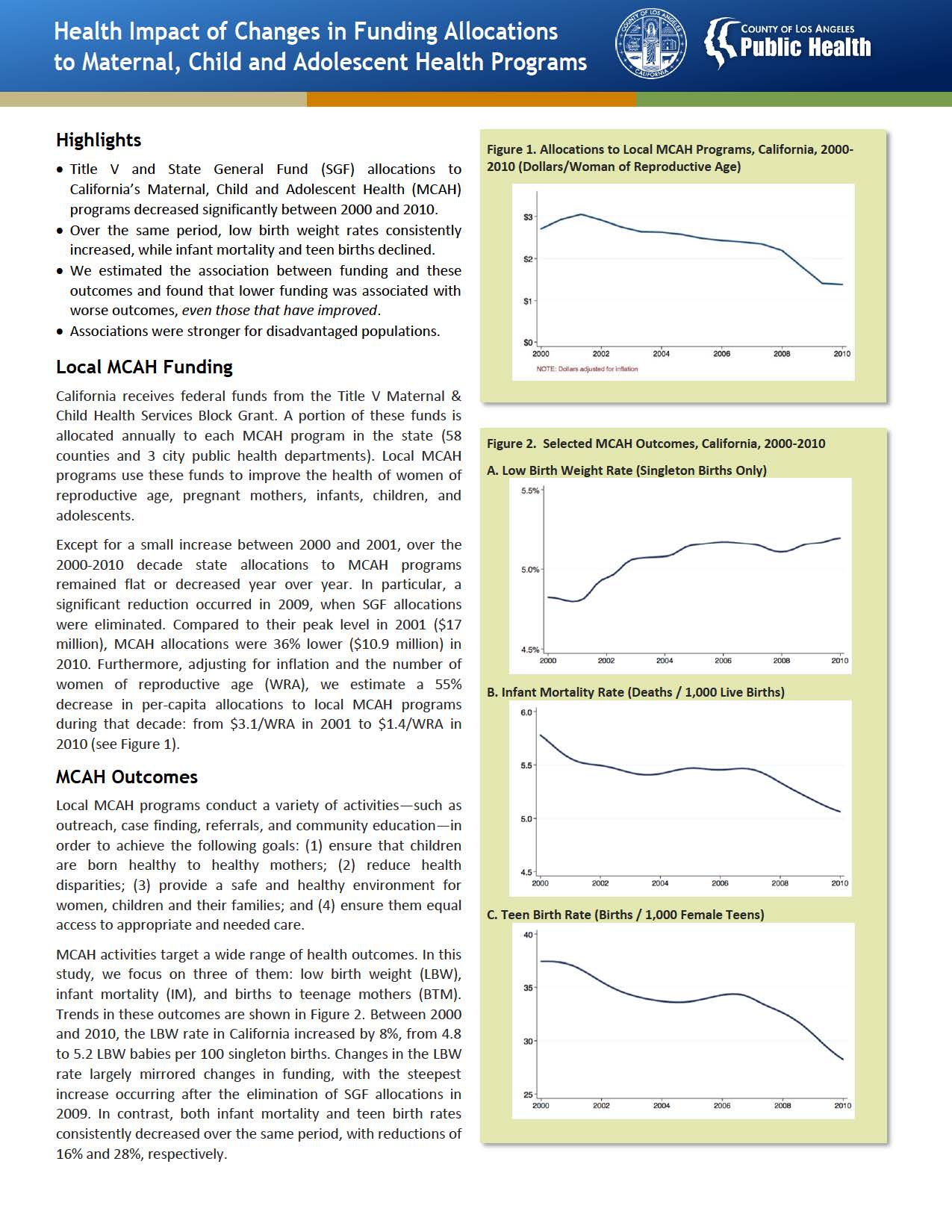
Issue Brief: Maternal, Child and Adolescent Health Funding
Health Impact of Changes in Funding Allocations to Maternal, Child and Adolescent
Health Programs (November 2014)
This was a collaboration with the Division of Maternal, Child and Adolescent Health.
Title V and State General Fund (SGF) allocations to California's Maternal, Child and Adolescent Health (MCAH) programs decreased significantly between 2000 and 2010. The objective of this study was to quantify how these funding changes have affected health outcomes. More specifically, we focused on low birth weight (LBW), infant mortality (IM), and births to teen mothers (BTM). We found that lower funding was associated with worse outcomes, even for IM and BTM, which have improved in recent years in the state, suggesting that MCAH funding reductions partially explain the recent increase in LBW rates and that IM and BTM rates could have improved even more in the absence of these funding reductions. Using the results of this analysis, we projected the potential impact of restoring funding to its peak level in 2001. For additional details on this study's methodology and findings, click the link below.
Rapid Health Impact Assessment: Parks After Dark
Potential Costs and Health Benefits of Parks After Dark
(September 2014)
This was a collaboration with the Division of Chronic Disease and Injury Prevention.
In collaboration with the Division of Chronic Disease and Injury Prevention (CDIP)
and the Center for Health Impact Evaluation, we conducted a rapid health impact
assessment (RHIA) of the Los Angeles County Parks After Dark (PAD) program. PAD,
initially a violence prevention strategy of the County's Gang Violence Reduction
Initiative at three parks, has evolved into a cross-sector collaboration offering a
gamut of recreational programs, cultural and educational activities, youth leadership
opportunities, and health services. The objective of this HIA was to inform decision
making by examining three alternative planning options: 1) continue PAD
programming as is, 2) expand PAD to include additional parks, or 3) discontinue PAD.
The rapid HIA made 9 overall recommendations to maximize potential health
benefits of PAD.
Rapid Health Impact Assessment: Parks After Dark Report
![]()
Cost Analysis: Shared Use Agreements in Los Angeles County
Impact of Shared-Use Agreement Adoption on School District Expenditures in Los
Angeles County
(August 2014)
This was a collaboration with the Division of Chronic Disease and Injury Prevention.
This study was one of three components led by CDIP; CHIE attempted to estimate the impact of shared-use agreement (SUA) adoption on school districts' expenditures. Shared-Use Agreements allow community members to access school facilities outside regular school hours. We compiled a dataset of SUA adoptions over the period of 2005- 2012 by school districts in Los Angeles County (LAC), focusing on SUAs that allowed the use of facilities for physical activity, and used California's Standardized Account Code Structure (SACS) data to track several types of district level expenditures over the same period. The results of this study showed that each additional school with a SUA was associated with $15,500 higher community services expenditures (p<.001) and $58,900 higher enterprise expenditures (p=0.10). For more information about the design, methodology and results, click the link below.
Cost Analysis: Shared Use Agreements in Los Angeles County Report
![]()
Rapid Health Impact Assessment: The Potential Costs and Benefits of Providing Free Public Transportation Passes to Students
The Potential Costs and Benefits of Providing Free Public Transportation Passes to
Students in Los Angeles County
(October 2013)
This was a collaboration with the Division of Chronic Disease and Injury Prevention, who led the
project.
The Los Angeles County Department of Public Health (DPH) conducted a rapid health impact assessment (RHIA) of the costs and benefits of providing free transit passes for all students from preschool to college, regardless of income. To inform decision making, DPH focused its assessment on the program's costs and benefits, and identified priorities by key stakeholders and decision-makers in the community. The Center for Health Impact Evaluation assisted CDIP with the cost calculations. For detailed information about potential costs, conclusions and recommendations, click the link below.