This webpage is designed for the public and healthcare professionals to share information and resources addressing false information
and to help build trust and confidence in life saving vaccines.
Introduction
Page Updated 10-27-25
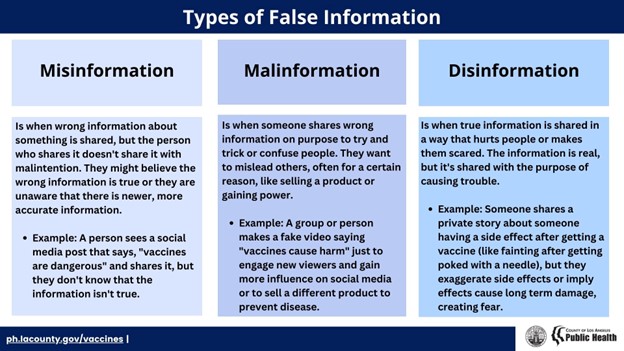
- False information poses a serious threat to public health and well-being.
- False information can lead people to believe things that aren’t true, influencing them to make decisions that may put their health or their loved one's health at risk.
- False information can create unnecessary fear and hesitation about life-saving vaccines.
- Unverified health claims and rumors spread rapidly, fueling distrust in medical experts and public health institutions.
- Staying informed with accurate information is essential for protecting yourself, your family, and your community from preventable diseases.
We want to hear from you! Click here to submit vaccine questions you have or to share false information you may have encountered. A staff member of the LAC DPH vaccine preventable disease control program will address your feedback.
Appendix, & Resources
General Resources:
- lacounty.gov/vaccines (LAC DPH) - FAQs available in multiple languages
- Health Media Literacy Checklist (LAC DPH)
- Vaccinate Your Family
- This website provides clear, reliable information about vaccines and the diseases they prevent to help the public make informed decisions about vaccination.
- Evaluating Health Information (UCSF Health)
- Disinformation (Voices for Vaccines)
- Vaccine Confidence Toolkit (Association of Immunization Managers)
Vaccine Education Resources:
- The Complete Guide to Childhood Immunizations -
(American Academy of Pediatrics)
- This video course provides new parents with a comprehensive understanding of childhood vaccinations, explaining the importance, recommended schedule, and the diseases they protect against, along with the potential risks of not following the vaccination guidelines.
- UNITY® Consortium Podcast
- This podcast is centered around “myth-busting” commonly held misconceptions surrounding vaccines – particularly adolescent and young adult vaccines.
References
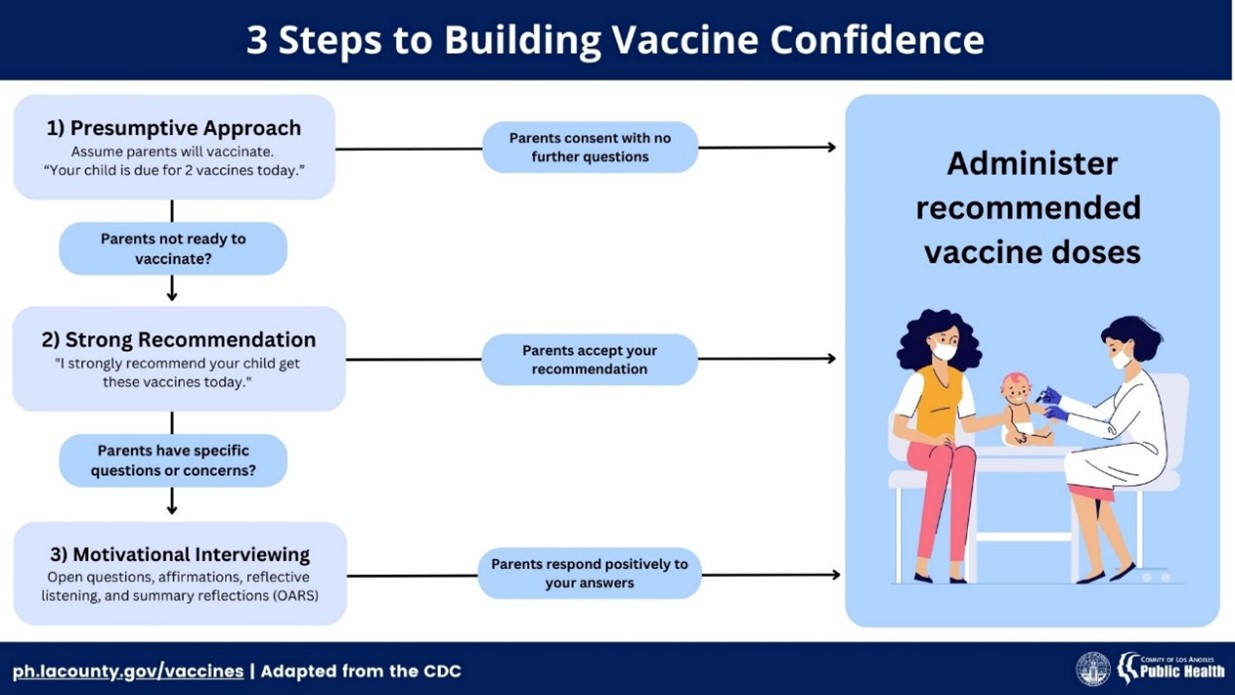
- O’Leary, S. T., Opel, D. J., Cataldi, J. R., Hackell, J. M., O’Leary, S. T., Campbell, J. D., Ardura, M. I., Banerjee, R., Bryant, K. A., Caserta, M. T., Frenck, R., Gerber, J. S., John, C. C., Kourtis, A. P., Myers, A., Pannaraj, P., Ratner, A. J., Shah, S. S., Kimberlin, D. W., . . . Emanuel, A. (2024). Strategies for improving vaccine communication and uptake. PEDIATRICS, 153(3). https://doi.org/10.1542/peds.2023-065483
- Centers for Disease Control and Prevention. (n.d.). Conversation tips for healthcare professionals: Vaccines and children. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines-children/hcp/conversation-tips/index.html
- Gust, D., Brown, C., Sheedy, K., Hibbs, B., Weaver, D., & Nowak, G. (2005). Immunization Attitudes and Beliefs among Parents: Beyond a dichotomous perspective. American Journal of Health Behavior, 29(1), 81–92. https://doi.org/10.5993/ajhb.29.1.7
- Leask, J., Kinnersley, P., Jackson, C., Cheater, F., Bedford, H., & Rowles, G. (2012). Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics, 12(1). https://doi.org/10.1186/1471-2431-12-154
- Tuckerman, J., Kaufman, J., & Danchin, M. (2022). Effective approaches to combat vaccine hesitancy. The Pediatric Infectious Disease Journal, 41(5), e243–e245. https://doi.org/10.1097/inf.0000000000003499
- Centers for Disease Control and Prevention. (2024). Give a Strong Vaccine Recommendation. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines-children/hcp/conversation-tips/index.html
- Steward, E. E. & Fox, C. (2011). Encouraging Patients to Change Unhealthy Behaviors With Motivational Interviewing. American Academy Family Physicians (AAFP). https://www.aafp.org/pubs/fpm/issues/2011/0500/p21.html
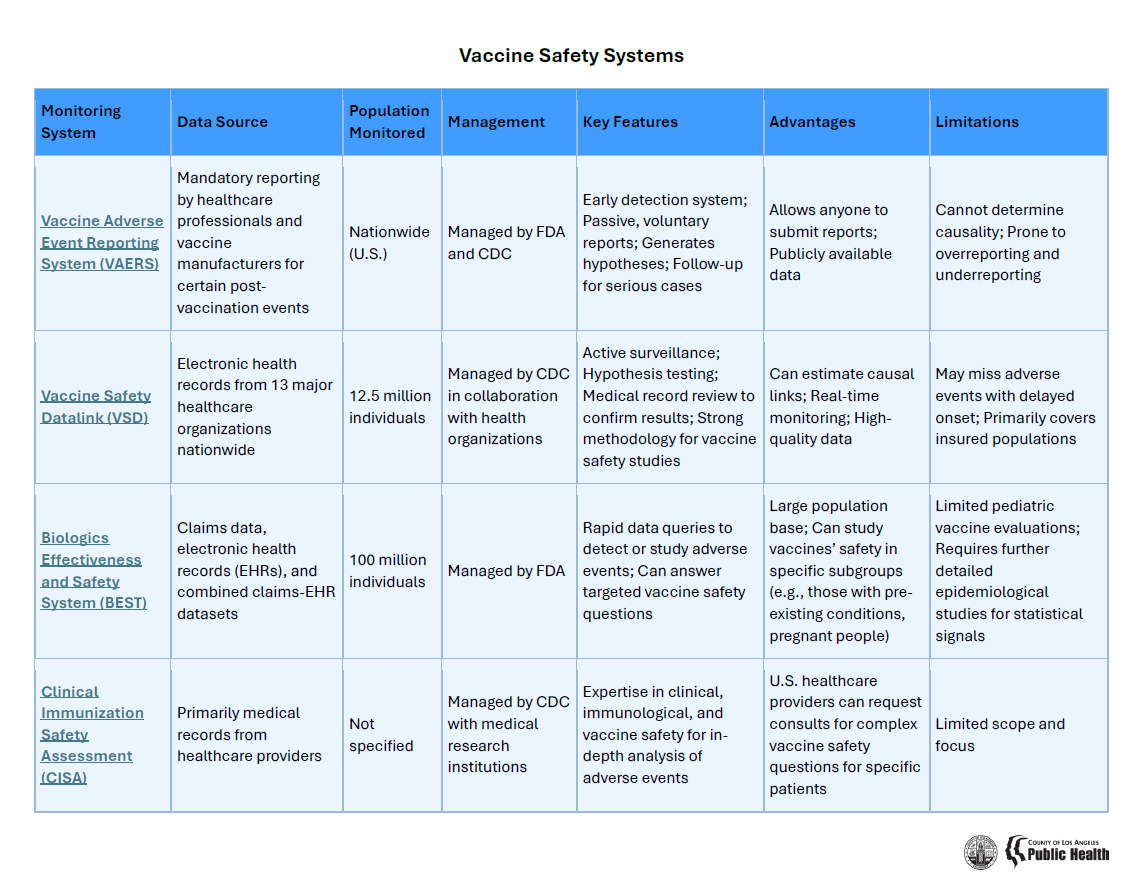
- Developing Safe and Effective Vaccines. (2024). Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines-children/about/developing-safe-effective-vaccines.html
- Vaccine Safety: Examine the Evidence. (n.d.) healthychildren. https://www.healthychildren.org/English/safety-prevention/immunizations/Pages/Vaccine-Studies-Examine-the-Evidence.aspx
- Taylor, L. E., Swerdfeger, A. L., & Eslick, G. D. (2014). Vaccines are not associated with autism: an evidence-based meta-analysis of case-control and cohort studies. Vaccine, 32(29), 3623–3629. https://doi.org/10.1016/j.vaccine.2014.04.085
- Los Angeles County Department of Public Health. (2023). Vaccine Misinformation. Los Angeles County Department of Public Health. ph.lacounty.gov/ip/docs/vaccine-misinfo/VaccineMisinformation.pdf
- Zeinstra, H. (2025). Common myths about vaccination. Unity Consortium. https://www.unity4teenvax.org/resource/common-myths-about-vaccination/
- Vashishtha, V. M., & Kumar, P. (2024). The durability of vaccine-induced protection: an overview. Expert Review of Vaccines, 23(1), 389–408. https://doi.org/10.1080/14760584.2024.2331065