Syndromic
Surveillance in
Los Angeles County
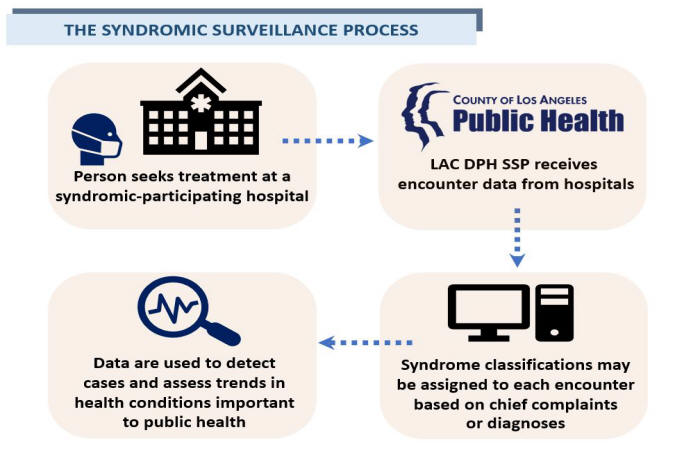
Syndromic surveillance is a population-based early detection and monitoring system that uses data collected in near real-time from emergency departments and other clinical (e.g., nurse telephone triage) and non-clinical (e.g., over-the-counter drug sales) sources. This public health tool aids traditional surveillance by providing timely awareness of disease trends through the analysis of existing health data for unusual increases in syndromes.
The Los Angeles County Department of Public Health (LAC DPH) Syndromic Surveillance Project (SSP) has accepted Admit-Discharge-Transfer (ADT) data submissions from hospitals with emergency departments (EDs) since 2002, and now collects data on more than 2.5 million encounters every year as reported by 80% of hospitals with EDs throughout the county, or 91% of all ED encounters. The ADT messages are snippets that contain limited demographic, chief complaint, diagnosis, admission, and discharge disposition information that are triggered as the patient progresses through certain points or actions initiated during their encounter. Once received, LAC DPH performs key word searches on the chief complaint and diagnosis information. The ADT messages do not contain the breadth and accuracy of information contained in a complete patient medical chart. However, the timely assessment of these pre-diagnostic and diagnostic data have provided a vital component to LAC DPH's emerging event detection capabilities, as well as situational awareness of various public health conditions.
In Los Angeles County, common uses of data include:
- Tracking community spread of emerging diseases and conditions (e.g., COVID-like illness)
- Monitoring seasonal patterns of diseases (e.g., influenza-like illness)
- Case detection (e.g., Multisystem Inflammatory Syndrome in Children, Acute Flaccid Myelitis, meningococcal disease)
- Evaluating health outcomes related to an environmental event (e.g., respiratory symptoms during wildfire season, heat-related illness during a heat advisory)
- Monitoring trends in non-communicable illnesses (e.g., vaping use-associated lung injury)
- Surveillance of mass gathering events (e.g., Special Olympics)
Important Considerations when interpreting Syndromic data
Syndromic surveillance data are not meant to represent the true number of cases of a disease in a population, but can be used to look at disease trends by the percentage of visits over time. Additional considerations include:
- Syndromic participation over time - The number of syndromic participating hospitals has increased over the years, leading to improved coverage and higher ED volume. When interpreting trends across the years, comparing counts should be avoided.
- Geographical coverage - ED access and utilization patterns may vary across the county. For instance, residents close to the border of another county may be more likely to seek care in that county; information on these visits are not transmitted to the SSP. Spatial comparisons should be done with caution.
- Changing ED visitation patterns - Emergency department visitation patterns may change based on the day of the week (weekends versus weekdays, for instance), on major holidays, or other circumstances. Typically, we utilize percentages rather than counts in order to take into account shifts in overall ED volume - the implied assumption here is that the percentage of misclassified or underreported cases is fixed over time. More recently, however, ED volumes were observed to have dropped by more than 40% for a period of time estimated to be between March 2020 through June 2021, due to changing ED visitation patterns during the COVID-19 pandemic. In addition to a drop in overall volume, there was also a shift in the distribution of the health conditions for which ED patients were seeking treatment as the general public was advised to avoid seeking care at hospitals when possible in order to accommodate surges of COVID-19 patients. One cannot make the assumption of fixed percentage misclassification and underreporting during this period of shifted ED utilization; careful consideration should be made when doing time period comparisons.
- Quality - The quality of SSP submissions from hospitals has improved as reporting standards have become more comprehensive and also as hospitals have modernized their systems to be able to transmit more of the required data elements and workflows. The SSP accommodates upgrades to existing connections on an ongoing basis in order to accommodate hospital EHR system modifications as well as to bring the collection of data elements and workflows to current messaging guide standards; however, there remains variability between hospitals in what data elements hospitals are able to send.
- Completeness - Visits are classified into syndrome
categories based on chief complaints and/or coded
diagnosis. There is however variability in the quality
and collection of chief complaint and diagnoses across
syndromic participating hospitals. Chief complaint is
often recorded as a free text field and may contain
misspellings and abbreviations. It may also be a limited
field or picked from a drop-down menu in some
facilities. Some hospitals can map only one chief
complaint value into the Syndromic ADT message even
though the patient is experiencing a variety of
symptoms. Similarly, some facilities are only able to
submit a fixed number of diagnosis values, or a subset
of diagnosis types; some facilities are not able to
submit any diagnosis codes at all, at this time. As a
result, the reason for visit information pertaining to
each encounter received through Syndromic Surveillance
is almost always incomplete. The implications here are
that:
- Even with perfectly crafted search term lists, the counts and percentages of encounters classified into each syndrome category will always be underreported.
- The absence of certain chief complaint or diagnosis terms should never be interpreted as an absence of a health condition.
- Special consideration should be made when defining syndrome categories requiring more than one symptom or key word.
- Misclassification - Free text fields may contain words, parts of words, or abbreviations that are unintentionally or incorrectly picked up in key word searches, leading to misclassified or incorrect detections. For instance, CHF is an abbreviation for Crimean hemorrhagic fever, but also for congestive heart failure. Search terms used to track wildfire-related ED encounters may include the word "fire" - but this may also pick up unrelated references to "fire station", "fireplace", "firework", "fire alarm", "fire department" and even "hamburger and fires".
- Diagnostic delay - Diagnosis data may take a few days to weeks to come in, so interpretation of recent trends should be done with care.
- Illnesses with common search terms - Health conditions with search terms that are shared with another health condition - especially a health condition more commonly presented at the ED during the time period assessed -- may be poor candidates for a Syndromic use case. For example, a search for pertussis-related ED encounters during influenza season is not a great application because there are typically many more cases of respiratory conditions other than pertussis circulating in the population by two or three or more orders of magnitude; and because the main pertussis symptoms of cough and fever and shortness of breath are shared with these other more common respiratory conditions. As a result, any true pertussis trend may be undetectable above the "noise" of day-to-day variation in unrelated detections.
- Rare conditions - Health conditions which are rare and/or spread out over time and/or may involve a wide variety of symptoms may also not be detectable over background data noise. The best use cases therefore, are those that have specific search terms not applicable to other health conditions or situations (e.g., "gun shot", "lettuce"), and/or have assigned ICD10 code (e.g., U07.1 for diagnosed COVID). However, even if the search terms are not unique to other health conditions, a large enough increase in cases for the health condition assessed over a short amount of time may still be detectable above background noise.
Participation in LAC DPH's Syndromic Surveillance Project
LAC DPH is able to accept syndromic surveillance data reporting from eligible hospitals (EHs) and critical access hospitals (CAHs) to contribute to the Center for Medicare and Medicaid Services (CMS) regulatory requirements of the Public Health and Clinical Data Exchange objective for the Promoting Interoperability (PI) Program and the Merit-based Incentive Payment System (MIPS) (PDF) Eligible hospitals for PI are defined as acute care hospitals (including CAHs and cancer hospitals) with at least a 10 percent Medicaid patient volume, and children’s hospitals (no Medicaid patient volume requirements).
LAC DPH is the public health agency for required Promoting Interoperability reporting in Los Angeles County. To meet the federal PI public health syndromic surveillance requirements, all ED-receiving EHs and CAHs in Los Angeles County must report and electronically submit the appropriate data for syndromic surveillance directly to LAC DPH.
LAC DPH's SSP is currently onboarding new hospital connections. Eligible hospitals and critical access hospitals must be ED-receiving and operating in Los Angeles County; connections with private providers or medical groups cannot be accommodated at this time.
- Hospitals may contact lacphsynd@ph.lacounty.gov to begin the active engagement process. The SSP will provide a letter of attestation for this activity upon request. Due to high demand, the hospital may be placed in a temporary hold queue.
- Hospitals that are currently participating in the LAC DPH Syndromic Surveillance project, and are looking to upgrade their data connections, should also email lacphsynd@ph.lacounty.gov for further assistance.
- For all other eligible providers, please take the exemption for this measure as we are only taking registration for EHs and CAHs. For your records, please print out the documents made available on the http://www.publichealth.lacounty.gov/cdcp/meaningfuluse.htm website.
LAC DPH's Syndromic Surveillance Project (SSP) is in the process of onboarding with the National Syndromic Surveillance Program (NSSP) to contribute LAC DPH syndromic data to the NSSP BioSense Platform, a secure integrated electronic health information system. NSSP is a collaboration among the CDC, public health agencies, and partners with the aim of advancing the timely exchange and use of syndromic data. The BioSense platform enables aggregation and analysis of syndromic data which can be used to provide local, regional, and national awareness of various public health conditions.
For concerns about your facility's data being shared with the NSSP, please contact the SSP at lacphsynd@ph.lacounty.gov within 30 days of registration.